Ignore health scares, HRT is safe, say scientists
Hormone Replacement Therapy is safe, scientist have concluded, and one million women have been suffering debilitating symptoms of menopause needlessly because of flawed reports linking it to cancer.
Hormone Replacement Therapy is safe, scientists have concluded, and one million women may have been suffering debilitating symptoms of menopause needlessly because of flawed reports linking it to cancer.An entire generation of women stopped taking HRT following studies in the early 2000s which suggested that the treatment raised the risk of heart disease and breast, ovarian and womb cancers. But new research, which followed women for a decade has found no evidence that HRT is linked to any life-threatening condition. It means that for more than a decade, a million post-menopausal women have been enduring hot flushes, night sweats, depression and increased risk of osteoporosis for no reason. Dr Lila Nachtigall, a professor of obstetrics and gynaecology at New York University, said it was a "shame" that there had been a "huge drop" in the number of women taking HRT following health scares. "We found women taking HRT over a long period of time to be in very good health," she said.
"It's now clear that women on HRT over many years can enjoy benefits. The risks of HRT have definitely been overstated. The benefits outweigh the risks."
HRT, which boosts levels of the female hormones oestrogen and progesterone, was developed in the 1940s and was first made available to women in Britain in 1965. However by the mid 1990s concern was growing about the drugs and two large studies were launched, one in the US and one in Britain.
In 2003 the British Millennium Women Study published its findings claiming that HRT raised the risk of cancer. Many doctors immediately withdrew prescriptions while the Medical Healthcare and Regulatory Agency (MHRA) issued new guidance recommending all women be given the 'lowest effective dose should be used for the shortest time.'
Within four years the number of women taking the hormones had plummeted from two million to one million. Although later studies cast doubt on the original findings, and Danish research found HRT may even lower the risk of heart disease, the numbers of women taking the drugs never recovered.
The new study by New York University school of medicine tracked 80 women using hormone replacement for 10 years and compared them with a control group who were not using the medication. The HRT group suffered no more incidences of cancer, diabetes or heart disease than the control group.
Health experts in Britain said that many doctors were still confused by the research and were frightened to recommend HRT despite the wide benefits. Many women suffering symptoms are currently prescribed anti-depressants.
Professor John Studd, consultant gynaecologist at the London PMS and Menopause Clinic, said: "The problem is that most GPs are frightened of HRT – they will have learned as medical students that it is linked to health risks, and it sticks in their minds.
"But those studies that were replicated in the textbooks were worthless – they were completely rubbish. They collected the data all wrong.
"HRT has huge benefits in terms of relief of menopausal symptoms – there is less depression and women feel better."
A separate poll released today by HRT makers Mylan revealed that 85 per cent of women who could benefit from the treatment are not taking them, one in four because of health fears.
Dr Sarah Gray, a Cornwall GP and women’s health specialist, added: "Women are currently reluctant to seek help for their daily symptoms due to confusion over the role and safety of HRT. "This means that many women may be unnecessarily experiencing symptoms that are impairing their quality of life on a daily basis. "Women need to know about the available options, their risks and benefits and be empowered to become part of the decision-making process. "In the past, many menopausal women with low moods have turned to anti-depressants or anxiety medication, when an effective alternative might be HRT."
Nick Panay, consultant gynaecologist at Queen Charlotte's & Chelsea and Chelsea & Westminster Hospitals, said: "We believe that the tide is turning. "There were certain risks shown by the WHI (Women’s Health Initiative) study, but observational studies before that and other studies since have been much more reassuring. It seems that the problem with the WHI study was that the HRT doses used were too high and many women were well beyond the average age of menopause at 51.
"We believe that the right HRT preparation, in the right woman, has low overall risks and has significant benefits.
"Too many women are being denied hormone therapy that might benefit from it. Where there are risk factors, it is about properly risk assessing women on an individual basis."Menopause should be taken seriously and women should be given the opportunity to use hormone therapy when appropriate to do so."
Nice is planning to launch the first guidelines into the treatment of the menopause in November. The new research was published at the ASRM annual meeting in Baltimore.
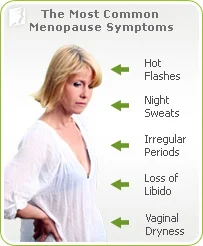
Menopause Symptoms
As women enter their 40s and 50s, there are a number of changes going on within their bodies. Each woman will experience a different menopause, but becoming knowledgeable about the signs, symptoms, and treatment options is the first step
As women enter their 40s and 50s, there are a number of changes going on within their bodies. Each woman will experience a different menopause, but becoming knowledgeable about the signs, symptoms, and treatment options is the first step to ensuring that you manage your menopause — rather than it managing you. Your “survival kit” is knowledge paired with action.
Knowledge: Some symptoms that may be a part of your menopause include: Hot flashes; rapid heartbeat; irritability, mood swings, sudden bouts of crying; trouble sleeping loss of libido; crashing fatigue; incontinence; breast tenderness; depression; weight gain; hair loss (or thinning); and increased facial hair.
Knowledge:
The phases of menopause include:
- Perimenopause: This is the time leading up to menopause when your body begins producing less of hormones like estrogen and progesterone. As a result, women begin to lose their ability to become pregnant. Symptoms may begin as early as 35, but often begin between 45 and 55.
- Menopause: Your period stops and perimenopause symptoms may increase. Menopause is defined as 12 consecutive months without a period (and there are no other causes).
- Post-menopause: Most of the menopausal changes have faded. Hot flashes may seem milder or less frequent; energy and emotional levels may seem to have stabilized. Bone loss and estrogen loss are areas of concern.
Action:
- Relieve the symptoms by keeping a journal to record changes and anticipate changes. Watch for food triggers like spicy foods or heavier meals.
- Dress in layers so you can easily cool down if a hot flash attacks.
- Focus on your health and improve where you can — stop smoking, start exercising.
- Some alternative therapies, such as acupuncture, may have results for some women.
- Counseling or support groups are an option for women struggling with the changes in their bodies and the associated lifestyle changes.
- Hormone replacement therapy (HRT) can be discussed with your physician if more moderate changes in diet, exercise, and supplements do not offer the level of treatment desired.
Vaginal estrogen linked to improved sexual health for some women
Among women who don’t take hormonal replacement therapy (HRT) after menopause, and even some who do, vaginally applied estrogen may help ease dryness and painful intercourse, a small U.S. study suggests.
Among women who don’t take hormonal replacement therapy (HRT) after menopause, and even some who do, vaginally applied estrogen may help ease dryness and painful intercourse, a small U.S. study suggests. Women were most likely to use the vaginal estrogen if they reported pain during sex, and if they had stopped HRT, the study found.
Among the women who abandoned HRT and never went back, the participants using vaginal estrogen reported significantly higher satisfaction with their sex lives, the study published in Menopause also found.
“We would expect that the women with the most severe symptoms would show the greatest benefit and the group that stopped estrogen/hormone use after the WHI would be expected to develop symptoms and benefited the most,” senior study author Dr. Michelle Warren, of Columbia University Medical Center and the Center for Menopause, Hormonal Disorders and Women’s Health in New York, said by email. Women go through menopause when they stop menstruating, which typically happens between ages 45 and 55. As the ovaries curb production of the hormones estrogen and progesterone in the years leading up to menopause and afterwards, women can experience symptoms ranging from irregular periods and vaginal dryness to mood swings and insomnia.
Vaginal dryness and painful intercourse are symptoms thought to result from atrophy of vaginal tissues because of falling estrogen levels. HRT has been shown to improve these symptoms by rebuilding vaginal walls.
For the study, Warren and colleagues studied vaginal estrogen use and sexual health in 310 women in New York City who were born between 1938 and 1953 and had used HRT for at least five years.
While about 36 percent of women who stopped HRT used vaginal estrogen, so did around 17 percent of women who continued HRT, the study found.
Overall, roughly a quarter of women in the study used vaginal estrogen.
The researchers acknowledge that the study is limited by its small size and the fact that participants were generally healthy, highly educated women with normal weight, so the results may not generalize to other groups.
Even so, the findings suggest that some women may benefit from vaginal estrogen whether or not they use HRT, the authors conclude.
“Vaginal estrogen is safer because very little if any estradiol gets into the blood stream,” Dr. Michael Thomas, a researcher in reproductive endocrinology and infertility at the University of Cincinnati Medical Center, said by email.
Lubricants may help make sex less painful for women after menopause, but this alternative can’t work like estrogen to improve the mucous lining of the vagina and make bleeding and abrasions or tearing less likely during intercourse, added Thomas, who wasn’t involved in the study.